 Can You Join the Military if You Have Diabetes?
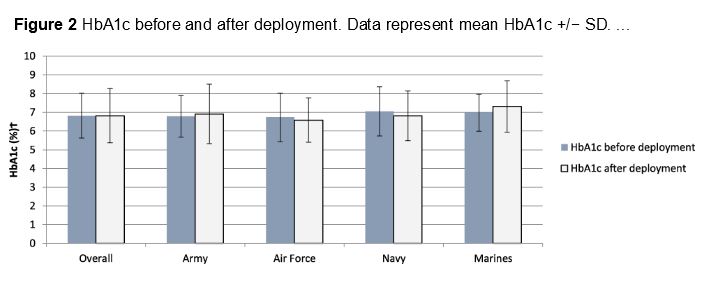
Can You Join the Military if You Have Diabetes?Warning: The NCBI website requires JavaScript to operate. Soldiers of the United States Army with type 1 MellitusY. Sammy Choi1 Department of Medicine, Womack Army Medical Center, Fort Bragg, NC, USA2Department of Research, Womack Army Medical Center, Fort Bragg, NC, USA3Department of Pediatrics, Womack Army Medical Center, Fort Bragg, NC, USAJon Cucura1Department of Medicine, Womack Army Medical Center, Fort Bragg, NC, USAAbstractUS Army soldiers diagnosed with type 1 diabetes were previously considered unfit by duty. For highly motivated soldiers, current advanced technologies allow the the possibility of maintaining active service not only, but of military deployment. We present our experience in Fort Bragg, North Carolina, caring for soldiers newly diagnosed with type 1 diabetes mellitus. Through intensive diabetes education, extensive military and physical training, diabetes optimization real-time remote control and technology, soldiers can follow Serve your country in the most specialized functions. When a United States Army soldier is diagnosed with type 1 diabetes, it is widely assumed that will be found unfit for duty and his military career is over. Previously, the rigors of unpredictable lifestyle and intense physical requirements prevent continuation in active service. But for a select group of highly motivated and qualified soldiers, it is possible to maintain active service. Fort Bragg, North Carolina, is home to some of the most skilled men and women in the many have spent years of education and intense operational training achieve your level of skill, experience and proven performance. When a soldier is diagnosed with type 1 diabetes, the Army can face a difficult decision. What should it be? made by an exceptionally qualified soldier who is also very motivated to remain active Service? How will hypoglycemia and hyperglycemia be handled? From a tactical point of view, the Commander of the unit has the responsibility to guarantee not only the security of the soldier with diabetes, but to ensure the safety of the entire unit. A soldier of withdrawal allocation due to a medical complication could significantly affect the unit mission. Army regulations stipulate that any soldier with diabetes who requires medications glycemic control will be referred to a Medical Evaluation Board (MEB) to determine the the capacity of the soldier to serve in active service. Many are found unfit for duty, ending their military careers. We have shown that it is possible not only to retain but also to preserve deploy soldiers with type 1 diabetes. Although not all soldiers deploy, our goal is to meet all deployment criteria 6 months from diagnosis (). In addition, all soldiers pass the physical examination of the Army and successfully complete other unit-related activities to demonstrate that the continuation of activities duty and deployment will be safe. Ultimately, it is the Commander's decision not only deploy but use any soldier. Therefore, close collaboration between the soldier, medical equipment, and unit is required every time it is implemented or any other activity is considered. Even when a soldier's military obligation ends, this search for aggression The benchmarks for safe deployment criteria prepare the soldier for success in the future life strives. Table 1. Orientation on the deployment of soldiers with Diabetes. FactorOK to deploy Should not be deployedHbA1c (for the patient)In target No discrimination on the basis of sex PresentationAsentment Autonomic NeuropathyBeforeRecognition of the rules of the sick day EnoughInsufficientProliferative diabetic retinopathyLoudPresentmentEdemaMacularAssyPoor hypoglycemia (An episode that requires another person) Infrequent history of diabetic cetoacidosis in 6 months agoNoYes Self-management skills GoodPoorHypoglycemia desconscience AbsentPresentParameters of permanent profile can be followed YesNoSignificant comorbidities (e.g., congestive heart failure, chronic kidney disease, significant coronary disease, disease Controlled hypertension) that requires intensive handling AbsentPresentThe noise of hypoglycemia is high if the NoSiDuty meals are lost or delayed, will place the soldier in an isolated area of OCONUS where adequate medical care and means to monitor and support it NoSource: Army Regulation 40-501, Table 5-. OCONUS, Continental United States. Soldier General Needs The preparation of military duty includes attention to specific tasks of events, as well as sleep, nutrition and hydration. We have used guidelines on sports nutrition promulgated by the American College of Sports Medicine and other professionals organizations, The type 1 diabetes soldier should maintain this energy fuel and proper glucemic control. Recommendations for athletes with type 1 diabetes are in according to the general guidelines for all athletes. This means acutely the prevention of hypoglycemia and the control of hyperglycemia that could lead to diabetic ketoacidosis (DKA). Such complications He could temporarily disable the soldier and put the unit at risk. Long-term, control means keeping an A1C suitable to minimize glucemic contribution Vascular disease. A more important long-term goal can be prevention of type 2 diabetes, as it is expected that approximately 40% of adults with type 1 diabetes develop type 2 physiology due to high prevalence of overweight and obesity in the United States. In a high-performance tempo environment, the latter is easy to overlook as soldier can be able to perform optimally without hypoglycemia or DKA, however with a suboptimal A1C. The challenge is to keep a soldier in conditions of service for the current mission success while avoiding future medical complications. Physical ActivityCivil athletes with type 1 diabetes currently compete in professional sports and resistance events, such as the Triathlon of Germany Ironman and others.- Maybe more remarkable to the community of diabetes is the success of professional cycling Team Novo Nordisk team. Such resistance events require tremendous preparation for any athlete safe. compete, and demand even more preparation for those with type 1 diabetes. Stop. soldiers who were formerly resistance athletes, we support the continuation of such activities. Our goal is to train carefully and optimize maximum performance. In Also, for those who do not participate in such activities, we encourage participation in other difficult persecutions beyond the physical fitness of the army test requirements. Successful completion within established glycosmic limits provides confidence to fulfill all military duties. In order to achieve militaryly relevant training, strict attention is paid to multiple factors required. As required for safe deployment, we highlight prevention sustained hypoglycemia/hyperglycemia, reliable monitoring and communication with the medical team. The optimal target glucose during the activity is 100-180 mg/dl and available several excellent reviews providing guidance on management the athlete with type 1 diabetes.- Ultimately, it is through Postgraduate activities and careful monitoring of a business management plan adapted to the metabolic signature and unique lifestyle of each soldier. Use of available technologies Established guidelines and our previous experience provide a model for business planning. Considerations include rest/dormitory effect, caffeine, diet type (e.g., pizza), environmental temperatures and the most important activity (type, intensity, duration, frequency). Previously, we require each soldier to perform self-monitoring of blood glucose (SMBG) 6-10 or more times a day to properly evaluate the effect of these and other variables. Remote electronic downloads facilitated easy information exchange, however Several tests were cumbersome due to SMBG impracticity during the activities. Use of revolutionized tests of ongoing real-time glucose monitoring for our Soldiers and now is a prerequisite to completing our training program. We currently use Diabetes Medtronicas, Northridge, CA, USA and Dexcom G5® (Dexcom, San Diego, CA, USA) systems for continuous monitoring of glucose. Sensors allow almost simultaneous verification of the initial and bolt basal parameters. We asked. soldiers fast until casualties are expected. Such information is priceless as unexpected rapids can be inevitable. After the insulin pump configuration are calibrated, soldiers are instructed to use the sensor continuously and record as much detail as possible surrounding any event or activity. As alluded to before, being aware of the internal and external factors associated with the event you can build a "activity data base" from which you can make future decisions. A soldier in a 10-mile march with 45 pounds of equipment would notice variables such as day time, temperature, humidity, terrain and altitude, quantity sleep and rest, emotional state, fitness level to include reference heart rate, diet, hydration status and duration of the activity. We found there's no data substitution and immediate security feedback provided by the continuous Glucose sensors. In particular, Dexcom G5 is useful as it provides the capacity of our entire equipment to see glucose values in real time. As an example, when a soldier goes in a tempered 10 miles by road, the soldier, medical equipment and unitary assets are capable of remotely controls real-time values. We are able to communicate with an embeby medical team member and provide immediate information and suggestions for attention. We We encourage our soldiers to evaluate their values in real time, to take care of themselves decisions, and to communicate with our team 24 hours a day as the need arises. So immediate Feedback provides invaluable lessons learned, and through repeated and repeated practice communication, direct trust in our team becomes less important. During the first 1-2 months of training, we emphasize that soldiers must notify us immediately when sugars are below 70 mg/dl or more than 250 mg/dl. Though trained Soldiers have written plans of action, encourage immediate calls to strengthen the management decisions to achieve our number one priority of keeping sugars out of the Danger zone. Fort Bragg results For the last 25 years, we have taken care of hundreds of soldiers, since junior enlisted to senior general officials, with type 1 diabetes. Our service members have not only have they been held, but have been able to remain in their army Occupational specialty including assignments within the 82nd Airborne Division and Special Operations Command. They have completed training, as the challenge Survival, Evasion, Resistance and Escape Course. Our last 50 consecutive soldiers with type 1 diabetes recently diagnosed in Womack Army Medical Center provides a snapshot of our experience in Fort Bragg (). All soldiers they were immediately introduced into advanced technologies and most were placed in insulin pump and sensor within weeks of diagnosis. Intensive face-to-face training was performed within the first two weeks involving multiple visits with our diabetes team; Preferably our team sees them within 24 hours of diagnosis. Telehealth was used immediately after diagnosis and almost exclusively after the MEB process Started. A1C was obtained in diagnosis, MEB remission, and every 3 months until separation from the army and/or relocation. Active service soldiers with type 1 diabetes: administrative results. The average age was 29.3 years; all but two were men. The average follow-up time was 28.7 months. It means A1 C in the diagnosis and the final visit was 11.4 and 6.6, respectively (). The only one adverse events were hypoglycemia requiring assistance (one) and DKA (two, one drug abuse). The 18 soldiers who wished to remain in active service were withheld. Table 2.Fort Bragg Outcome: Average monitoring of 28.7 months. A1CTotal (N = 50)Retaineda (n = 18)Not retained (n = 32)MeanMedianMeanMedianDiagnosis11.411.111.0In the reference pump MEBb6.6 (1.8)c6.1 (5.0-13.3)d6.7 (1.3)6.6.6 (5.0-11.2)-116.6 (2.0)6.0 (5.2-13). glucose sensor (insulin pump or sensor is not a requirement for retention). Some soldiers used a bomb with suspension of the threshold but we didn't notice any difference in severe hypoglycemia less than 50. No soldier used the closure of Medtronic 670G loop system as military insurance did not allow use. Five soldiers had deployments. The deployment of one soldier was denied due to the unit requirement of a fixed hospital; this was not a factor in those who was deployed as long as access to equipment and medical care was available. Environmental extremes, such as temperatures Ã90oF, do not exclude the assigned activities or significantly affect glucose control. All soldiers successfully They completed their tours. There were no complications in any of the 18 soldiers except one that required assistance for hypoglycemia in an undeplomed environment. e-Consultation in remote locations By using various telemedicine sites effectively, we can communicate with you soldiers almost anywhere in the world. Although not all deployments are approved, we However, work to ensure that all soldiers and their units have the capacity to contact our medical team 24 hours a day in case a soldier is released for such assignment. In terms of control, maintenance or slight increase in A1C to reduce risk Hypoglycemia is preferred. An average glucose lower than the renal threshold during deployment is sufficient, for example, 170 mg/dl or A1C of approximately 7.5. We feel this slight elevation in the glucemic level, if it happens, is reasonable in a effort to prevent hypoglycemia. Telemedicine capabilities can be used in deployed or other remote environments in the in the same way as during the training period to provide immediate information to our soldiers if necessary. For example, identification of stress-induced hyperglycemia During deployment activities, it would be useful to mitigate future potential problems. The use of real-time monitoring and other telecommunications technologies allows medical equipment to connect with the soldier anywhere accessible by cell telephone; it is not common for a soldier to be in an isolated region for long periods of time without that access. Disturbing circumstances and team effort could arise the net provision for the deployment of any soldier for any soldier is necessary situation. Optimization of current technology allows us to provide the greatest opportunity for the unit commander to better use soldiers with type 1 diabetes. We can also train soldiers who were diagnosed elsewhere. For example, we recently trained a Special Forces soldier with type 1 diabetes who was sent to Fort Bragg for two days of temporary service for intensive and remote insulin therapy technology skills training. Now we regularly monitor this soldier using the Dexcom Follow App (Dexcom, San Diego, CA, USA). Likewise, we can continue monitor soldiers from Fort Bragg who are in conditions of service and then move to another location. With the cooperation of your local medical teams, we can continue fully diabetes cares for those who want this arrangement. Debate Our experience in Fort Bragg, North Carolina, does not reflect Defense Department policies or practices in other military installations. Rather we will describe our attempts in the optimization of the performance of soldiers and the preparation of the unit when soldiers, medical personnel and unit support are available. Individualization is Key. Every soldier and his military specialty, unit location, the training and deployment mission should be carefully considered. For example, they are concerns regarding information technology security for the use of sensor technology, Just real-time transmission to a medical team? Even if all current capacities are accessible, is generally in the best interests of the unit, especially during deployment to use a soldier with type 1 diabetes. What about the ends of Disgusting? For example, we had a welded bomb failure during deployment and we determined was due to dust / sand during a particular weather pattern; use of a shower bag solved the problem. What about resupply issues particularly in relation to to insulin in the improbable but possible event of capture by the enemy? Finally, it's the soldier able to maintain proper control to prevent complications? These are all the important and serious considerations that are made about one Basis per case involving the adoption of shared decisions between the soldier and his family, medical equipment and unit. Conclusion We describe possible approaches, but not necessarily practical or generalizable, for a Weld diagnosed with type 1 diabetes. None of this would be possible without current advanced technologies. Remote monitoring in real time in particular prepares the active service soldier for military duty and successful life activities. Use of these current technologies have allowed us to keep our best and motivated soldiers ready to serve their country when duty calls. Footnotes Abbreviations: DKA, diabetic ketoacidosis; MEB, Medical Evaluation Board; SMBG, self-control Glucose in blood. Note by the authors: The opinions expressed here are those of the authors and not necessarily reflect the official policy of the Department of Defense, Army Department, USA U.S. Army Medical Department or Government. Statement of Conflict Interests: The author(s) did not declare potential conflicts of interest with respect to investigation, authorship and/or publication of this article. Financing: The author received no financial support for the investigation, authorship and/or publication of this article. ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
Fighting in type 2 diabetes in the care of military and permanent diabetesPeople also ask members of services With uncontrolled diabetes Allowed ...Type 2 Diabetes and VA Disability Compensation TEN CCK LawDiabetes in the Military - Learning About Diabetes ← Diabetes Auto ...Five Questions on Diabetes in the Military with Dr. J. Pinsker The Diabetes VA Claim: How many forms of service are connected ...Diabetes Mellitus (Type II) - CompensationRisk of Diabetes in U.S. Military Service Members in Relation to ...Can you join the military if you have diabetes?[PDF] Diabetes Handbook for Active Duty Service Members - Navy MedicineRelated searches

Can You Join The Military With Diabetes? It's Possible
Can You Serve In The Military With Diabetes?
Petition · Department of Defense: Allowing Diabetics to serve in Non-Combat roles in military · Change.org
Can You Join the Military if You Have Diabetes?
Petition · Allow Diabetics to serve in non-combat positions in the military · Change.org
Medical Conditions That Can Keep You From Joining the Military | Military .com
Five Questions on Diabetes in the Military with Dr. J. Pinsker
Can You Join The Military With Diabetes? It's Possible
Can Diabetics Serve In The Military? - OurMilitary.com
Serving in the Military With Type 1 Diabetes - Meet Mark Thompson - Diabetes Connections
When You're Diagnosed as A Young Adult: In The Military | College Diabetes Network
Can You Join The Military With Diabetes? It's Possible
Military Service in Korea
Can Diabetics Join the Army?/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/DVXBHQFPTFCTLBWJ2Y6B3GILR4.jpg)
59-year-old Afghanistan veteran will report to Army basic training this summer/army-woman-and-man-walking-with-duffelss-533929305-574ba4115f9b5851654b7f8c.jpg)
False Statements on Recruiting Paperwork
Can You Serve In The Military With Diabetes?
Military Medical Waiver Guide: Waiver Process For All 5 Branches
DoD Revises Requirements for Continuous Glucose Monitoring Use - U.S. Medicine/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/RD2CVCNIEREPRCCIZXYK6A6LJY.jpg)
Updated guidance allows unhospitalized COVID-19 survivors to join the military
Can You Join The Military With Flat Feet? Yes, But There's A Catch (2020)/https://public-media.si-cdn.com/filer/b3/ad/b3ad0112-0e4e-4f9e-8863-0171b1577dc6/07_01_2014_miltary.jpg)
More Than Two Thirds of American Youth Aren't Good Enough for the Military, Says the Military | Smart News | Smithsonian Magazine
Can You Join the Military with ADHD?
Here's why most Americans can't join the military
Chronic Diseases and Military Readiness | CDC
American Diabetes Month: Awareness promotes prevention > Ramstein Air Base > Display/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/6CJY3SIUHRECFHVFMYRMXF4E6M.jpg)
Updated guidance allows unhospitalized COVID-19 survivors to join the military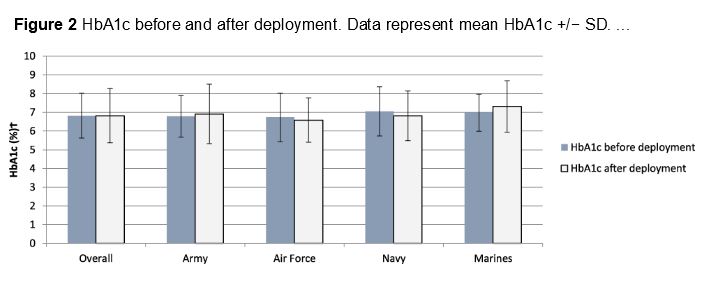
Servicemembers With Uncontrolled Diabetes Allowed to Remain In Military - U.S. Medicine
And I was going to apply for the marine band :( : diabetes_t1
Greek students frown at extended mandatory military service – EURACTIV.com
Does the National Guard Take Diabetics?
Can You Join the Military if You Have Diabetes?
Recruits with history of depression, bipolar disorder can get waivers to join Army: report | TheHill
Veterans and Diabetes: Diabetes Forecast®
DVIDS - News - Soldier serves in Kuwait, deals with diabetes daily
Join the Military or Go to College? You can Join the Military Reserve
Can You Join The Military With Type 1 Diabetes | DiabetesTalk.Net
Depression is not a symptom of weakness; it is treatable | Article | The United States Army
As Veterans Affairs Tests Keto Diet for Diabetic Patients, Skeptics Raise Red Flags | Healthiest Communities | US News
Why ADHD Restrictions for Military Service Are Unfair
 Can You Join the Military if You Have Diabetes?
Can You Join the Military if You Have Diabetes?













/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/DVXBHQFPTFCTLBWJ2Y6B3GILR4.jpg)
/army-woman-and-man-walking-with-duffelss-533929305-574ba4115f9b5851654b7f8c.jpg)



/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/RD2CVCNIEREPRCCIZXYK6A6LJY.jpg)

/https://public-media.si-cdn.com/filer/b3/ad/b3ad0112-0e4e-4f9e-8863-0171b1577dc6/07_01_2014_miltary.jpg)



/arc-anglerfish-arc2-prod-mco.s3.amazonaws.com/public/6CJY3SIUHRECFHVFMYRMXF4E6M.jpg)









Posting Komentar untuk "can diabetics serve in the military"